Around five years ago, I began a project with a District Health Board (DHB) to update its hospital’s aging BMS. The hospital in question is one of the world’s largest, so it was a challenge technically speaking, However, it also proved to be a valuable opportunity to disrupt the status quo. The project is now coming to an end, but the half-decade journey has revealed some significant flaws within the traditional approach. In this article, I explain the DHB’s process for redesigning their system along with how the project convinced me it’s time to rethink hospital building controls in general.
One District’s Journey
The DHB wanted to update its BMS after 25-years of service. But because it was a long-term investment, stakeholders wanted a progressive controls system, one that would align with future technologies and expectations around sustainability.
To design an innovative BMS that was forward looking and delivered better outcomes, the DHB needed a disruptive approach, one that challenged the status quo, identified old ideas, and replaced them with innovative thinking. To do that, it needed to examine how the building controls and health care industries had evolved over the last two decades—where they had been and where they were going.
Hospitals: From Commercial to Industrial
To say modern hospitals are different from those twenty-five years ago is an understatement. Today’s medical campuses are larger, their systems more integrated, equipment more complex, and standard of care much higher. In real ways, hospitals resemble manufacturing plants much more than large hotels. They’re just as industrial as they are commercial.
“Hospitals were complex, mixed-use facilities comprised of high and low-criticality systems.”
This is a critical point, because the standard approach to hospital controls is still heavily skewed to the commercial model. The industry’s commercial bias is unsurprising given the history of building controls.
After DDCs entered the market in the early 80’s, the big manufacturers used them to expand into the commercial sectors including hospitals. Being much cheaper than PLCs and designed for non-critical applications, DDCs were perfect for commercial facilities. Now, underserved sectors like hospitals could afford an all-in-one BMS solution that utilized these new controllers. This is still the standard approach for hospital controls.
However, today’s hospitals comprise many more industrial, mission-critical systems. To be sure, most campuses contain gift shops, florists, pharmacies, coffee shops and other commercial spaces. However, hospitals also house sophisticated operating theatres, large MRI machines, and industrial-grade boilers and chillers.
Hospitals are complex, mixed-use facilities comprised of both high and low-criticality systems, and the standard commercial approach often fails to address high-criticality needs.

Supporting Critical Services
It’s too simplistic to say a BMS only runs a hospital’s systems. That’s because without reliable systems, nothing else gets done. Like most facilities, hospitals require several key services to function properly. However, unlike typical commercial spaces, disruptions to basic utilities becomes a critical issue within hospitals.
For example, having no hot water heating services at an office building would result in complaints from bathroom visitors and coffee drinkers. At a hospital, lack of hot water services means patients can’t take showers, laundry workers can’t clean linen, emergency staff can’t properly wash their hands, and surgical instruments can’t be sterilized.
Without these basic utilities, many clinical services can no longer function. The BMS monitors and manages all these critical systems, so it too is a key supporter of clinical services. Yet, this supportive role is often overlooked when designing the resilience and reliability of a hospital’s building controls.
A New Approach
After consideration of changes within the BMS industry and the evolution of medical facilities, the district decided the standard controls model couldn’t ensure better outcomes for the hospital. To design a new fit-for-purpose model, the organization narrowed its focus to four key pillars:
- Criticality
- Security
- Lifecycle
- Procurement
Criticality
“Despite widely accepted use in most mission-critical facilities, medical building controls have traditionally failed to adopt PLCs for controlling boilers, chillers, and operating theatres.”
When it came to system criticality, the standard controls model proved too “flat”. In a flat design, every building system is assigned the same criticality level, and each is controlled by the same equipment. The result was a BMS that lacked nuance and flexibility. There was little nuance and flexibility for a high-tech medical facility that demanded both.
The flat design also left some systems under-engineered and others over-engineered. This prompted the district to reconsider their facility’s criticality levels. Overlaying the conventional DDC framework across the hospital’s non-critical commercial services no longer worked if those services were, in fact, high criticality.
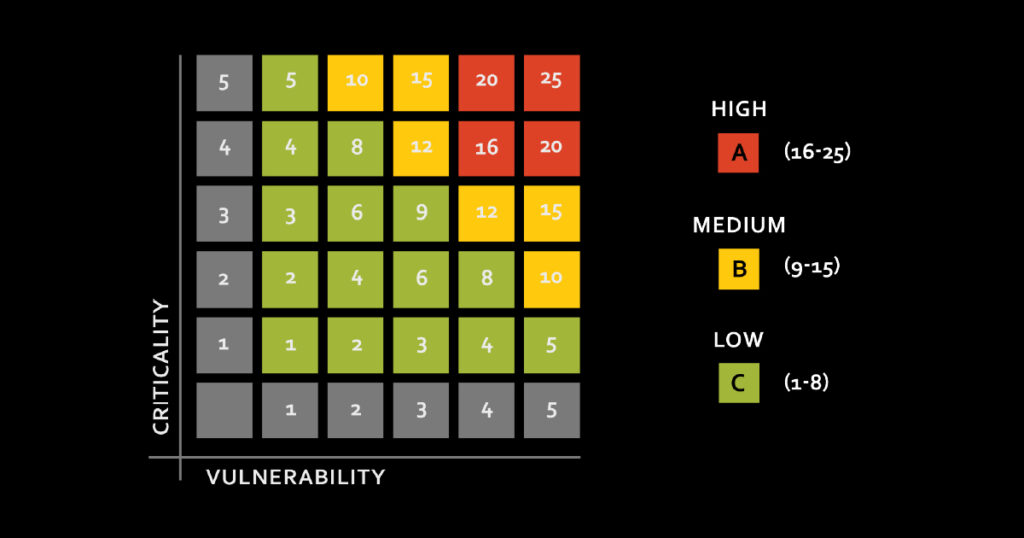
To address the issue, the DHB created a new criticality matrix, which expanded their criticality range from three categories to six. The change introduced finer gradations of risk levels into their design, countering the standard one-size-fits-all “flat” approach.
Next, the DHB looked for mismatches in criticality level and controller grade. It discovered several high-criticality services including operating theatres, MRI chillers and hot water plants were using commercial grade DDCs.
With the new information, stakeholders could now properly assign fit-for-purpose controllers to match risk assessments. This lowered costs while increasing system redundancy, resilience, and lifespan.
Finally, the DHB developed a naming convention based on the Brick schema. A standard naming convention would ensure efficiency and accuracy when storing and retrieving data and allow the hospital to take advantage of advanced data analytics.
Adopting a PLC Architecture
To address criticality mismatches, the DHB needed a fit for purpose controller that was robust and reliable. The PLC was the obvious choice. Despite widely accepted use in most mission-critical facilities, medical building controls have traditionally failed to adopt PLCs for controlling boilers, chillers, and operating theatres. Instead, these industrial-grade systems, which affect hundreds of patients, continues to be designed using the same commercial grade, non-mission critical DDC technology.
“Using PLCs gave the DHB a better tool for matching controller quality to their new criticality matrix.”
Programmable logic controllers come in a wide choice of models for a variety of system applications, ranging from business-critical M172s to life-safety critical M580s. So, using them gave the DHB a better tool for matching controller quality to their new criticality matrix. Plus, two decades of advances in controller technology had significantly reduced their price. They were now a feasible option.
However, as the DHB would learn, PLCs also came with many other benefits that would make them the best solution for disrupting the standard model.
Security
The DHB also needed to rethink the standard approach to network security. It ultimately found the traditional approach produced an ad hoc security that didn’t deliver on key outcomes.
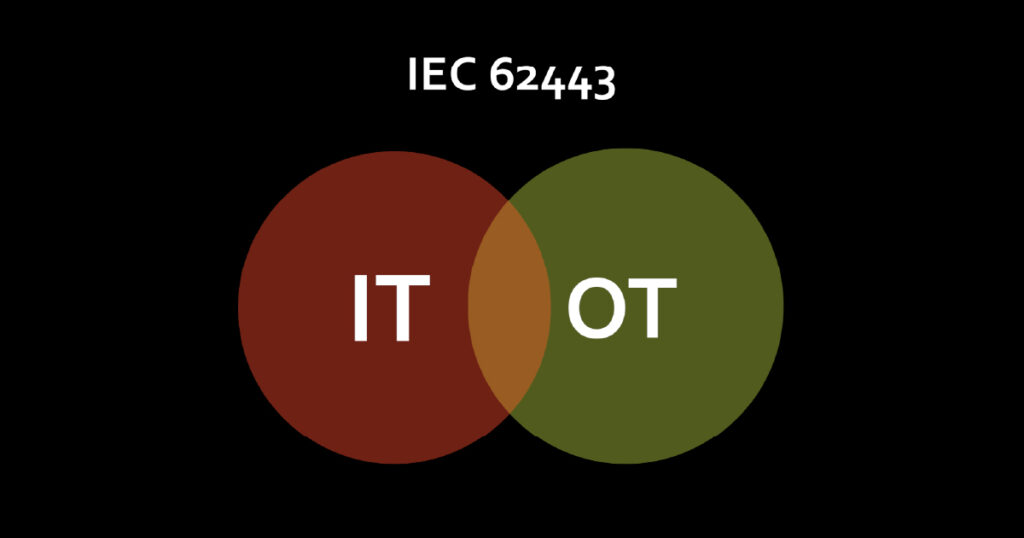
For one, networks and equipment lacked recognized protocol standards for communication. This meant there was little coordination between operational technology (OT) and information technology (IT). The lack of standards left both systems vulnerable to attack and network failure.
But because PLCs supported internal communication standards like IEC 62443, both IT and OT could use the same standards to coordinate their cybersecurity strategies.
The DHB found login security an issue too. Current usernames were generic or non-descriptive, and passwords were weak and easy to guess. To address login credential issues, the district standardized usernames and created complex passwords for users.
Lifecycle
Compared to PLCs, which have a lifecycle of at least 25 years, the DDC’s shorter lifespan (15 years) meant they needed replaced more frequently. PLCs are also more accurate, and have a higher-resolution I/O. They are battle-tested and go through extensive evaluation periods to ensure their accuracy and reliability. This makes them much more fault tolerant than DDCs. High criticality PLCs can also support dual processors and dual power supplies, which increases their resiliency. Overall, these qualities would extend the lifecycle of the hospital’s BMS.
Procurement
The DHB found that their current controls solution was highly customized to the hospital facility. Being boutique required more time and larger budgets for repairs and updates.
Again, the answer was programmable logic controllers. Since PLCs used open, non-proprietary standards for programming languages, any technician with knowledge of the standard could make changes to the BMS. PLCs would ensure a broader choice of vendors and suppliers. More suppliers also guarded against supply chain issues for replacement parts. And local vendor options could reduce lead times for maintenance.
In the end, the DHB determined that adopting PLCs would transform the standard model by moving the hospital from a single vendor to multiple vendors, from proprietary software to open software, from maintenance contracts to flexible contracts, from a boutique solution to a standard one and from limited choices to many.
Conclusion
My experience has taught me a change is needed in how the industry approaches hospital building controls. Large medical facilities have evolved, yet our approach to their controls hasn’t. Exacerbating the situation is the fact that the pace of change itself is accelerating.
Fast approaching sustainability mandates will soon require FMs to meet new expectations for efficiency and green energy use. Building automation, the Internet of Things, cloud computing and artificial intelligence are completely transforming how medical facilities operate.
It’s imperative we meet this challenge by discarding antiquated views and matching our system designs to the high functionality that modern hospitals demand.


One Response